Palliative Care Service consult pager: (917) 632-6906 or page 9399
Starting Dose for Opioid Naive Patients
Mild Pain: Non-opioids: acetaminophen 650-1000 mg PO q6h and /or ibuprofen 200-800 mg PO q6h should be tried first. Daily acetaminophen dose should not exceed 4 g/day in the adult, 3 g/day in the elderly, or 2 g/day in those with underlying hepatic dysfunction.
Moderate/ Severe Pain: Opioid +/- a co-analgesic. Starting doses are morphine 15-30 mg PO q4h, OXYcodone 10-20 mg PO q4h, HYDROmorphone 4-8 mg PO q4h. Co-analgesics such as acetaminophen, NSAID, anticonvulsants, antidepressants, and corticosteroids should be considered. * avoid morphine in renal dysfunction
Patients who are already taking opioids will require higher doses to control new or worsening pain. When the pain is NOT expected to resolve shortly, medications should be administered “around the clock” and additional “prn” or “rescue” doses should be available for breakthrough pain. Prescribe the standing medication based on its half-life (3-4 hours for short-acting opioids) and the rescue dose based on the time to onset (15-30 minutes for parenteral and 1 hour for oral).
Opioid Titration
For moderate pain, titrate the opioid dose at least every 24 hours. For severe pain, titrate more frequently. Increase the dose by 25-50% for mild to moderate pain, or by 50-100% for moderate to severe pain. Short-acting strong opioids (morphine, HYDROmorphone, and OXYcodone) should be used to control moderate and severe pain. Long-acting preparations (e.g. sustained-release preparations of morphine or OXYcodone or transdermal fentanyl) should be started after the pain is controlled on short-acting opioids. Never use long-acting opioids to control acute pain.
PRN dosing for breakthrough pain (i.e. acute pain in patients with otherwise controlled pain): give short-acting opioids using approximately 10% of the total 24 hour standing opioid dose, available q 1-2 h (e.g., patient on long- acting morphine 60 mg PO q 12h, breakthrough dose = short acting morphine 15 mg PO q1h prn).
Patient Controlled Anesthesia
PCA is a safe and effective method for delivery of opioids for pain that is expected to resolve (e.g., post-operative pain) and for acute exacerbations of chronic pain (e.g., pathologic fracture in a patient with chronic pain from bone metastases). Overdose is very infrequent because the patient must be alert in order to press the button.
Bowel Regimen
Patients on opioid therapy need an individualized bowel regimen prescribed prophylactically at the time of initiation, and continued for the duration of the opioid therapy. Maintain a high index of suspicion for bowel obstruction or fecal impaction. Rule out impaction with digital rectal exam or abdominal x-ray if clinically suspicious. Rectal disimpaction must occur before treating with an oral laxative.
- STEP 1: Docusate 100 mg PO tid plus Senna 2 tabs PO at bedtime. (Can titrate up to 8 Senna/day)
- STEP 2: Add Lactulose (or Sorbitol) 30 ml PO q24h. (Can titrate up to every 6 hrs)
- STEP 3: If constipated for 3 or more days, add Bisacodyl suppository (10 mg q24h), Docusate mini-enema at bedtime (Docusate, PEG, Glycerine), Fleet mineral oil retention enema, or Sodium phosphate oral sol, 30 ml PO. If no results, add a high colonic tap water enema (nursing order).
Opioid Overdose
Naloxone (Narcan) should be used only for life-threatening opioid-induced respiratory depression, an exceedingly rare occurrence in patients on chronic stable opioid doses. In order to minimize symptoms of opioid withdrawal (agitation, fever, emesis, and pain) when naloxone is needed, dilute 1 ampule (0.4 mg) with Normal Saline to a total volume of 10ml (1ml = 0.04 mg) and administer 1 ml IV q 1 min prn. This careful titration will reverse respiratory depression without causing withdrawal. The half-life of naloxone (1 hour) is shorter than the half-life of opioid agonists; therefore additional doses or a continuous infusion of naloxone may be needed
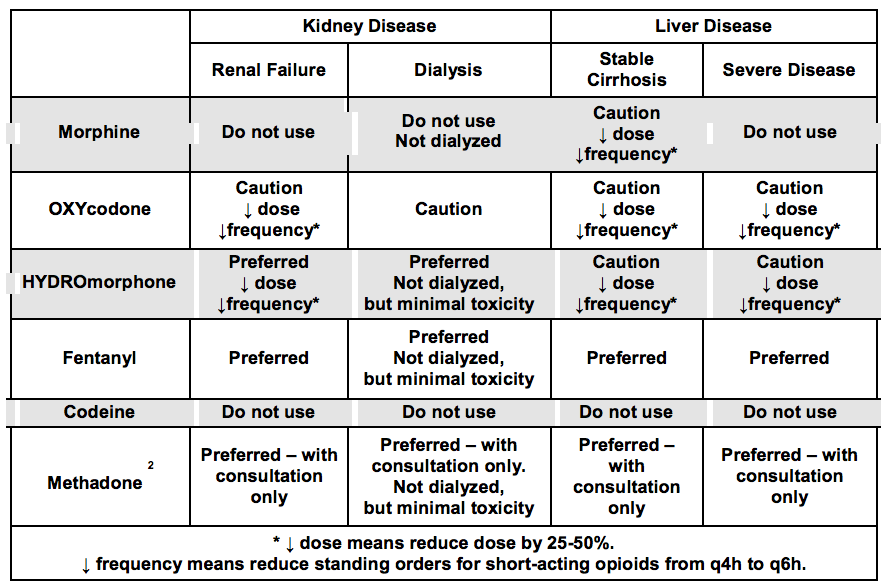
Opioids in Kidney and Liver Diseases
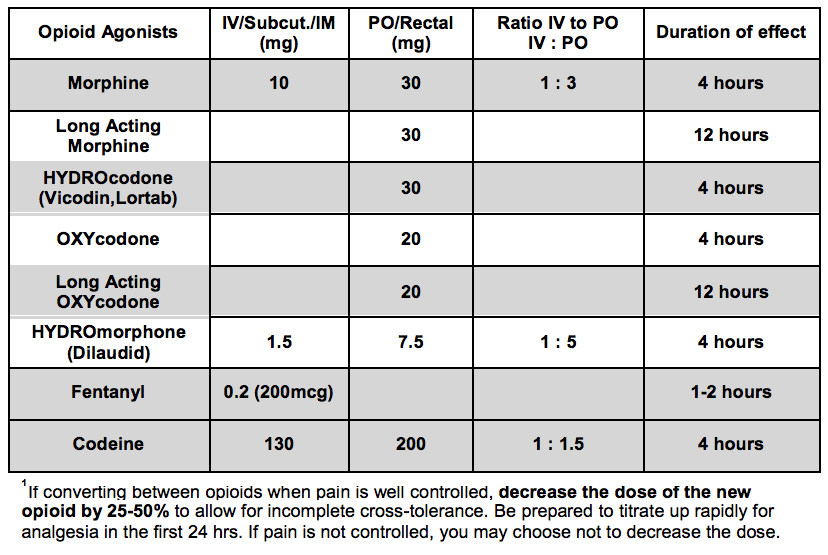
Opioid Analgesic Equivalences